Lyme disease and other tick-borne illnesses have reached epidemic proportions in Connecticut and in much of the United States. One of the greatest difficulties facing patients and physicians is that Lyme disease rarely presents with the classic symptoms reported in medical textbooks. Rather, Lyme has been called the new “Great Imitator” because it can look like almost any other disease and commonly looks like several different diseases at the same time. Historically, Syphillis was the first “great imitator.”
In this article, we will review some Lyme Basics, including what Lyme is, how people get it, how physicians make the diagnosis of Lyme disease and how it is commonly treated. We will also review the less well-known but more common presentations of acute and chronic Lyme disease, symptoms in children (as children act much differently than adults when they are infected with Lyme disease), and individualized approaches to treatment.
Lyme Basics
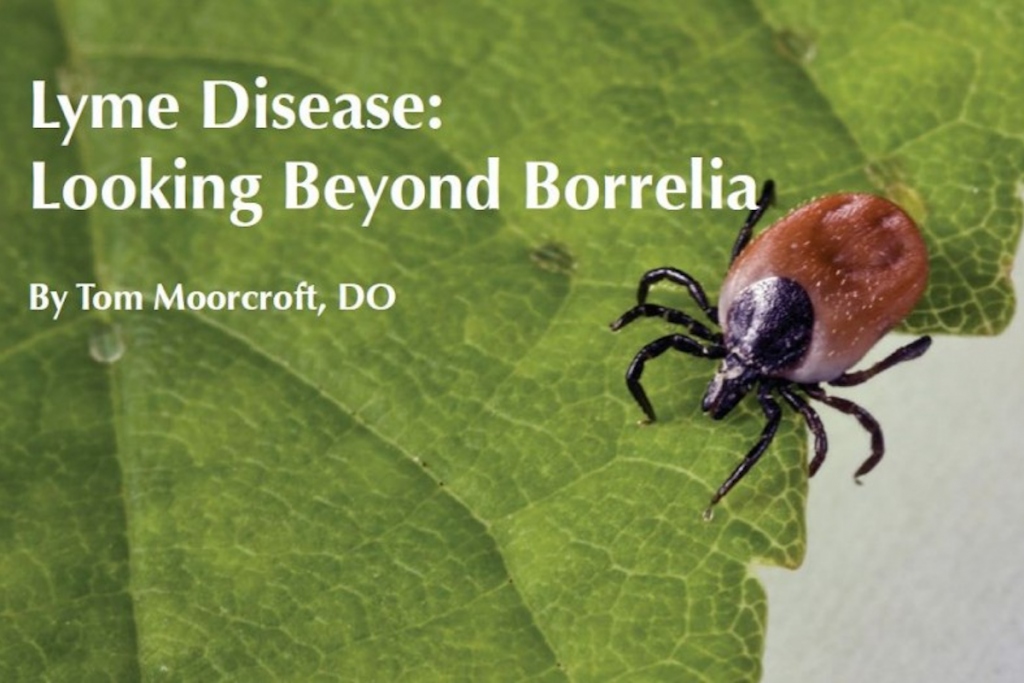
Lyme disease is the most common vector-borne disease in the United States. It is transmitted to humans by the bite of an infected Ixodes scapularis tick. This tick is better known by its common name the blacklegged or deer tick. Lyme disease is caused by the bacterial spirochete Borrelia burgdorferi. Cases of Lyme have been reported in all 50 states. Summer is the peak time for people to get deer tick bites , but since symptoms may not show themselves for 1-3 months or more after transmission, it’s important to keep Lyme in mind year round.
Deer ticks can be active during all months of the year; however, peak incidence of Lyme transmission occurs during the summer months. Adult deer-tick activity peaks in early spring and again in mid-fall. Adult ticks account for transmission of about 5% of reported cases of Lyme disease. The much smaller nymphal tick, that is about the size of a poppy seed, is responsible for about 95% of cases of Lyme and is most active from mid-May through late August in Connecticut. However, I’ve personally seen nymphs active in Connecticut as late as October.
Nymphal ticks feed for 4 days while adult ticks feed for 5-7 days. The rate of transmission of Lyme from the bite of an infected tick increases over time. Transmission over the first 48 hours is about 12%, however it increases dramatically to 75% at 72 hours and 94% at 96 hours.
The Centers for Disease Control and Prevention (CDC) has indicated that reported cases of Lyme disease are about 10% of actual cases that meet their surveillance criteria. This means that up to 90% of cases that meet these criteria are not being reported. Currently, more than 20,000 cases of Lyme disease are being reported each year in the United States. If unreported cases are as prevalent as suspected, then there are likely more than 200,000 new cases per year. This would mean that each year 5 times more people would contract Lyme than HIV/AIDS.
Lyme disease has reached epidemic proportions in the Northeastern states, including Connecticut. In 2009, the Connecticut statewide incidence of Lyme disease was 122 cases per 100,000 people, with some counties reaching a rate of 252 cases per 100,000. This is a startling increase when compared to the 2004 statewide incidence of 40 per 100,000. If CDC estimates are correct that would mean that approximately 1 in 100 people in Connecticut become infected with Lyme disease each year. Approximately 25% of the people who become infected with Lyme are children.
Symptoms of Lyme Disease
A red rash with central clearing (bull’s eye), called erythema migrans (EM), is diagnostic of Lyme disease. Studies show that 40-69% of people have the classic EM rash; however, physicians report that this rate may be as low as 10%. This rash may not occur at the bite site. Patients may present with multiple EM rashes or other types of rashes. Fifty to seventy-five percent of those infected with Lyme disease do not remember having had a tick bite.
Lyme is a complex, multi-system disease that has the potential to affect every organ system in the body. The most common symptoms of acute Lyme disease include flu-like symptoms, migratory joint and muscle pains, fatigue, headache, cognitive dysfunction (often called brain fog) and migratory paresthesias (a numb or tingly feeling). Some patients experience sound and light sensitivity as well as eye pain.
Because Lyme can present with many different, seemingly unrelated symptoms, patients may be misdiagnosed with conditions including depression, anxiety, migraine headaches, fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome and leaky gut, Parkinson’s disease, and multiple sclerosis. Severe cases of Lyme can cause heart block (a blockage in the heart’s electrical system), meningitis (inflammation of the covering of the brain and spinal cord) or encephalitis (inflammation of the brain itself), amongst other problems. More than 350 medical conditions have been noted to be caused or associated with Lyme disease in peer-reviewed medical journals. Early detection and treatment can help prevent the late manifestations of Lyme that are often severe and difficult to treat.
Children and Lyme Disease
Children under the age of 15 account for 25% of reported cases of Lyme disease. While some children present with the more common features of Lyme disease that we have already discussed, many of them present in ways that are much different than adults. Many children develop sleep problems, including nightmares. New onset bedwetting may also develop. Daytime urinary frequency is often seen. Some children present with odd skin sensations, others with discomfort when being touched. They often complain of headaches that can range from mild to debilitating. Commonly, children present with isolated neuropsychiatric and gastrointestinal changes. This makes the diagnosis of Lyme disease in children more challenging as well as more crucial.
Neuropsychiatric changes can range from mild to downright scary to parents and teachers. Children may experience acute changes in personality, abrupt behavioral changes, uncharacteristic outbursts, and trouble tolerating their normal environment. Some children have outbursts of rage; this is often directed at one family member or schoolmate. Children may also have problems with speech and motor skills leading to rapidly declining grades. Difficulty in processing auditory input often appears as a lack of focus leading a child to be misdiagnosed with attention deficit hyperactivity disorder (ADHD). Some children with Lyme disease develop problems with sensory integration and have a difficult time focusing when they are exposed to multiple stimuli at once. This leads to confusion and, in turn, poor behavior.
Happy children may become irritable and sad. Children may have an abrupt change in their mood to the point they are depressed, anxious, psychotic, and even suicidal. If this is the case, it is important to consider Lyme disease as well as co-infection with Bartonella henselae. Some previously outgoing and gregarious children become withdrawn or reluctant to play. Children may develop odd, repetitive behaviors and/or tics. When several of these symptoms are seen in the same child, they may be misdiagnosed with autism.
Children and adolescents often exhibit Lyme disease symptoms in the GI tract. These include abominal pain, heartburn, nausea, vomiting, diarrhea and blood in the stool. Gastrointestinal Lyme disease may mimic colitis or Crohn’s disease. Small intestinal bacteria overgrowth may be present. H. pylori is frequently resistant to treatment if Lyme disease is also present in the GI tract. Co-infections including babesia, bartonella, and mycoplasma, have been found in the GI tract.
Co-infections are other infections that can be transmitted by the bite of an infected tick. One common co-infection is Babesia microti. Babesia symptoms include sweats (day or night and often drenching), unrelenting headaches or head pressure, heart palpitations, a burning sensation in the feet, and muscle and bone pain. Ehrlichia and anaplasma are infections that can come on quickly and cause very high fevers, chills and intense fatigue, although they can also present as moderate headache and fatigue. In addition to neuropsychiatric changes, Bartonella hensalae can cause purple stretch marks and make stretch marks and surgical scars change from skin tone to a more purple color. When symptoms are all on one side of the body, Bartonella is often the culprit. These co-infections cause similar symptoms in adults.
Making the Diagnosis of Lyme Disease
The diagnosis of Lyme is often made using the criteria set forth in the CDC surveillance case definition of Lyme disease, including a two step laboratory testing strategy: an antibody screen followed by a confirmatory Western blot. These tests are known to miss 20-50% of patients who have Lyme disease. On its website, the CDC states, “This surveillance case definition was developed for national reporting of Lyme disease; it is not intended to be used in clinical diagnosis.” One of the biggest problems with Lyme-disease testing is that the best tests available are blood tests and Lyme disease does not live in the blood. Currently there are no blood tests that can tell your doctor that you do or do not have Lyme, they can only tell if
you have been exposed to Borrelia. Your clinical condition, supported by blood tests, is the only accurate measure of active Lyme disease. A negative blood test does not mean you do not have active Lyme disease; it may mean your immune system is not producing antibodies to Borrelia, it is up to your physician to determine if you have active infection. Lyme disease is a clinical diagnosis supported by blood tests.
In Connecticut, if your doctor is considering the diagnosis of Lyme disease, it very well may be the correct diagnosis. Studies have shown that in the Northeast, as many as 70% of ticks may be infected with Lyme and 50% of ticks may carry other tick-borne illnesses. In 2009, tick drags conducted by researchers at the University of New Haven found that a startling 90% of ticks carried Lyme disease and 30% carried Babesia microti.
Treatment of Lyme Disease
The best treatment for acute Lyme disease is antibiotics. The standard of care in the United States is 3 weeks of one antibiotic
and this is reported to cure Lyme disease. Unfortunately, this common assertion is inaccurate and contradictory to almost all scientific research done on Lyme disease. Research shows that the Lyme spirochete has many mechanisms by which it can hide from your immune system and live despite high doses of multiple antibiotics. There are several distinct forms of the spirochete, each of which requires a different type of treatment; unfortunately most doctors are only taught about one form. This means that many people who are treated for acute Lyme disease will be undertreated and go on to develop chronic symptoms.
Borrelia lives outside of cells and inside of cells. Some forms of Borrelia have cell walls and others do not. When exposed to a threat, such as antibiotics or herbs, the Borrelia spirochete can roll up into a protective ball called a cyst and remain dormant. Cysts generally open up to reproduce about once a month, however they have been reported to lie dormant in test tubes for 10 months or more before opening back up to become a fully active spirochete. Borrelia can kill white blood cells (immune cells that are attempting to protect you from the spirochete) and cover itself with their proteins; the body now views the spirochete as if it were a white blood cell, effectively cloaking it from your immune system. One of the other ways
Borrelia evades your immune system is called a biofilm. A biofilm is formed when many spirochetes group together and create a thick, gelatinous coating over themselves. We mau need to use antibiotic doses 1000 times higher than usual doses in order to penetrate biofilms. Since this is not practical or safe, we have had to come up with other methods of treatment to break up biofilms.
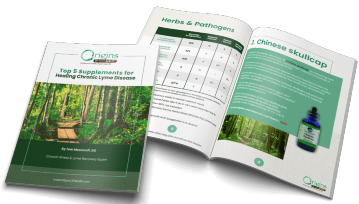
Patients who present with long-standing untreated or undertreated Lyme disease have several different treatment options. They may be treated with multiple different antibiotics, multiple different herbals or a combination of antibiotics and herbs. Lyme disease significantly changes how all the body’s systems function, so patients with chronic Lyme disease often have many other problems that must be addressed. Some of the most common conditions that are induced by or worsened by Lyme disease include heavy metal toxicity, vitamin and mineral imbalances, and hormonee imbalances, including thyroid and adrenal dysfunction.
It has been my experience that Lyme disease is not only the new “Great Imitator,” but also that it is the “Great Instigator.” Lyme has a tendency to create all sorts of other problems and then hide in one of its dormant forms. Patients are left with many different symptoms that seem unrelated. They often are diagnosed with fibromyalgia, chronic fatigue syndrome and even a somatization disorder (a fancy way of saying all your symptoms are in your head). I have found that Lyme disease severely impacts one’s vitality. Many affected patients have little or no reserves remaining. Minor insults result in tremendous flares of symptoms and suffering. It is crucial for physicians seeing patients with Lyme disease to look at them as individuals who have multiple different stressors affecting them rather than focusing solely on Lyme disease.
Looking Beyond Borrelia
There are many toxins outside our bodies that are exerting negative forces upon us. If we are to remain healthy we must exert a force that is equal to or greater than those forces in response. When our bodies are in balance with all the things that are pushing in on us, we are able to maintain a state of health. When the force applied on us is too great, a state of imbalance results. Over that last thirty or so years, the amount of toxins bombarding our bodies has increased exponentially. On a day to day basis we are exposed to so many toxins that we are barely able to maintain a state of balance and health. Infection with Borrelia commonly initiates a domino effect and our once good health seems to fall apart nearly overnight.
When I evaluate patients I always apply the Chronic Toxin Overload model. This concept allows us to look at each person as a unique individual and fully evaluate the role of all the different toxins that are impacting him or her on a daily basis. It also helps us remember that the symptoms a patient is experiencing are the result of all the toxins they are exposed to in addition to their unique genetic makeup. Each patient needs to be treated as an individual who responds to insults on their health in a manner that is unique to them. This approach to diagnosis and treatment is rarely seen in conventional medicine because it requires spending time with patients, getting to know each one as an individual, and creating an individualized treatment plan.
I believe that Lyme disease is difficult to diagnose and treat for three main reasons:
- Borrelia is a complex organism that has developed many ways to evade detection by our immune systems.
- Borrelia is the Great Instigator. It decreases our vitality and modifies our internal environment in ways that cause subclinical failure of many of our body’s systems.
- Lyme disease is rarely the only toxin exerting a strong negative force on a patient.
The Chronic Toxin Overload model provides us with a framework that allows us to understand that one toxin is rarely the problem. It helps us understand why Lyme is not the only toxin impacting our patients and how it can function as an instigator of so many other problems. Additionally, we can see why so many patients with Lyme disease get so ill and continue suffering despite aggressive antibiotic or herbal treatments.
In today’s world of nuclear radiation, global warming, 4G phones, high-speed internet, high-stress jobs, mercury fillings, and unclear futures due to faltering economies, we are all under a tremendous burden of chronic toxins. Our world has changed significantly over the past several hundred years. In addition to ever-increasing toxic stresses, our environment is ever changing. Each time a forest is cut down to make room for a residential or commercial development, we create more prime tick habitat. Our families are now forced live and play in areas where ticks are likely to live. Lyme disease is no longer only a tick borne illness; it is a complex physical, mental, emotional and social condition that is very common, but unfortunately often goes undiagnosed.
Fortunately, patients are speaking up. By raising their voices their doctors are slowly beginning to listen. Many physicians are seeking additional training in the diagnosis and treatment of Lyme disease. Still others are integrating the use of conventional medications with herbal and nutritional treatments. It has been my experience that there is hope to end the suffering of patients with persistent Lyme disease. By looking at and addressing all the potential toxins affecting a person, chronic illness dissolves. When patients who are suffering are evaluated and treated as unique individuals, patients regain their health and their lives.