Infection with Bartonella has sparked a ton of controversy in the medical community. Most people know Bartonella henselae as the causative agent of cat scratch disease. In medical school, we’re taught that this disease is usually mild and self-limiting. It rarely needs treatment unless you’re quite unlucky or you are immunocompromised. So basically, for most of us, nothing to worry about.
Like Lyme disease, most doctors are taught about what happens “most of the time,” meaning to 60-70% of relatively healthy people who get the disease. But, what about the other 30-40%? In the case of Bartonella, this could be quite serious, like developing neuroretinitis or endocarditis. These are relatively rare and, when found, usually treated aggressively. Doctors generally pick up on these conditions due to their severity and, despite being rare, fit into a pattern we’ve been taught to look for.
Those who don’t fit the pattern
Are there times when patients have Bartonella infections and they don’t fit the common pattern of disease we were taught in school? Absolutely. In the Journal of Central Nervous System Disease, Dr. Breitschwerdt and colleagues published a case of a young man who developed acute neuropsychiatric symptoms, including psychosis. [1] Four psychiatric hospitalizations, multiple psychiatric medications treatment for autoimmune encephalitis failed to relieve his symptoms. Finally he was diagnosed and treated for probable Neurobartonellosis based upon his symptoms and presence of cutaneous skin lesions (often called tracks or striae).
Despite nearly 2 months of treatment with one of the “drugs of choice” for Bartonella infection, he remained symptomatic and Bartonella DNA was found in blood samples after special processing. The standard blood tests for Bartonella henselae were negative. Following this, he was treated with combination antibiotic therapy. His neuropsychiatric symptoms gradually resolved, he came off all psychiatric medications, the skin lesions resolved and he returned to his pre-illness state.
Some important points to bring up here:
Neovascularization
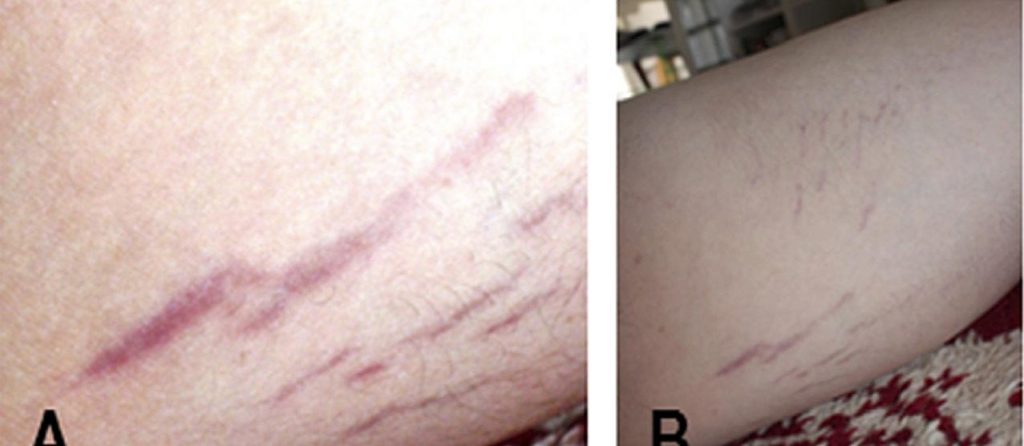
Bartonella henselae, quintana and bacilliformis have known to promote neovascularization – growth of new blood vessels from existing ones – in immunocompromised patients. So there has been the thought that skin tracks – purplish red stretch marks – that generally do not follow skin planes and are blanchable may be caused by Bartonella in immunocompetent patients exhibiting systemic symptoms consistent with Bartonella infection. Researchers have come very close to confirming this suspicion. [2] Clinically, when patients with these types of track marks are treated their symptoms generally improve and the tracks lose their purple-red coloration or resolve all together.
Bacterial resistance
Single antibiotic therapy, the most commonly recommended treatment approach next to no treatment, has been found to lead to bacterial resistance in laboratory studies. [3,4] This is consistent with what we see clinically. Multiple antibiotics or combinations of antibiotics and herbal therapies are generally necessary.
Bartonella persisters?
According to Dr. Li and his group at Johns Hopkins, “Bartonella henselae can cause various infections in humans, ranging from benign and self-limiting diseases to severe and life-threatening diseases as well as persistent infections that are difficult to treat.” [5] In their efforts to find better treatments for persistent Bartonella infections, they evaluated FDA-approved drugs against the stationary phase forms of Bartonella henselae. The two main forms are log growth or rapidly reproducing with increasing number of bacteria and stationary or slow reproducing to maintain a stable number of bacteria, but without population numbers increasing.
What they found was most commonly used drugs against the rapidly dividing forms of Bartonella henselae were ineffective against the stationary phase. And, the drugs that were effective have significant side effects and are not readily available (mainly because they are IV and need to be administered in a hospital setting). Fortunately, they found other, more readily available and easier to use drugs that were effective.
This study helps us understand two main things. 1. Bartonella infections have forms that can lead to persistence and 2. There are treatments that, at least in a science lab, work against these forms. Fortunately, the addition of medications to address the Bartonella stationary phase has been very effective in many of my colleague’s and my clinical practices.
Can Bartonella cause behavioral problems?
In this case, infection with Bartonella induced a type of autoimmune encephalitis called Pediatric Acute-Onset Neuropsychiatric Disorder (PANS). PANS is characterized by abrupt onset of cognitive, behavioral or neurological symptoms. These changes are commonly behavioral in nature where children develop acute OCD, rage, or anxiety and show significant regression, be it in school performance, social abilities and even bedwetting. Clinically, Bartonella can lead to symptoms such as OCD, tics, rage, regression and other oddities, even without triggering an autoimmune encephalitis.
How do you get Bartonella?
In addition to getting Bartonella henselae from cat scratches or bites, it has also been found in spiders and spider bites have been a proposed mechanism of transmission [citation]. There is controversy whether or not Bartonella is found in the same tick that gives you Lyme disease and, if it is, can the tick transmit it to you. Results of studies into both of these questions have been varied so there are no clear cut answers, however it is looking less likely that Bartonella is commonly present in deer ticks [citation, data from UMASS]. Other Bartonella species can be transmitted through flea and louse bites. Many parents of my patients are stunned when I ask them about lice and they recall their child’s behavior issues started shortly after an outbreak of lice at school. It’s not always clear cut how someone was exposed to Bartonella, but what is clear is I frequently find evidence of exposure to Bartonella and, with treatment, patients get better.
Awareness
This article is not meant to be an exhaustive discussion of human Bartonella infection. This is a really complex topic. Rather, I want you to be aware of the possibility that odd things happen and sometimes they are triggered by a treatable underlying cause. Early identification, diagnosis and treatment generally leads to the best outcomes.
Sources:
- Breitschwerdt E.B., Greenberg R., Maggi R.G., Mozayeni B.R., Lewis A., Bradley J.M. Bartonella henselae bloodstream infection in a boy with pediatric acute-onset neuropsychiatric syndrome. J. Cent. Nervous Syst. Dis. 2019;11 doi: 10.1177/1179573519832014.
- Maggi RG, Ericson M, Mascarelli PE, Bradley JM, Breitschwerdt EB. Bartonella henselae bacteremia in a mother and son potentially associated with tick exposure. Parasites & Vectors. 2013;6:101. doi:10.1186/1756-3305-6-101.
- Biswas S, Raoult D, Rolain J-M. Molecular Characterization of Resistance to Macrolides in Bartonella henselae. Antimicrobial Agents and Chemotherapy. 2006;50(9):3192-3193. doi:10.1128/AAC.00263-06.
- Rolain JM, Brouqui P, Koehler JE, Maguina C, Dolan MJ, Raoult D. Recommendations for Treatment of Human Infections Caused by Bartonella Antimicrobial Agents and Chemotherapy. 2004;48(6):1921-1933. doi:10.1128/AAC.48.6.1921-1933.2004.
- Li T, Feng J, Xiao S, Shi W, Sullivan D, Zhang Y. Identification of FDA-Approved Drugs with Activity against Stationary Phase Bartonella henselae. Antibiotics (Basel). 2019;8(2):50. Published 2019 Apr 29. doi:10.3390/antibiotics8020050